Metastatic breast cancer, a condition in which cancer cells have spread beyond the breast to other parts of the body, poses significant challenges in terms of treatment and patient prognosis. While conventional therapies like chemotherapy, radiation, and hormone therapy have been instrumental in managing this advanced stage of breast cancer, the emergence of immunotherapy has opened up new avenues for treatment. Immunotherapy harnesses the power of the immune system to target and destroy cancer cells, offering a promising alternative or complementary approach. In recent years, the field of immunotherapy drugs for metastatic breast cancer has gained considerable attention and research focus.
This article explores the exciting advancements and potential of immunotherapy in addressing metastatic breast cancer, focusing on the various types of immunotherapy drugs, their mechanisms of action, clinical trials, efficacy, and future directions in this rapidly evolving field.
Understanding Immunotherapy
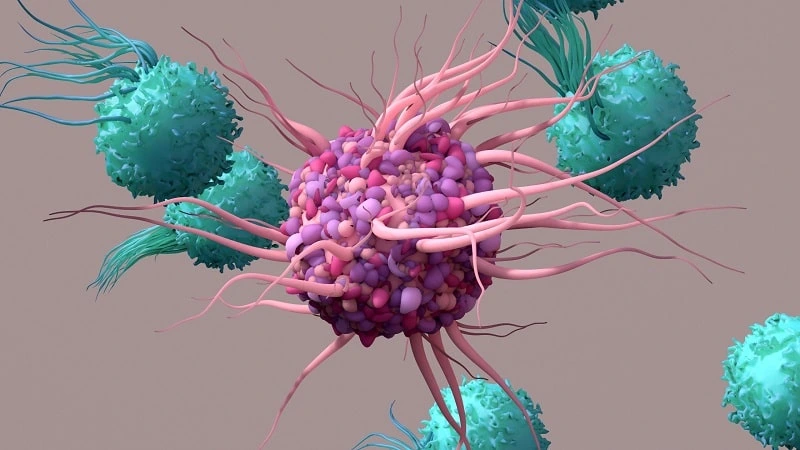
Immunotherapy, a groundbreaking approach in cancer treatment, harnesses the power of the immune system to recognize and attack cancer cells.
By stimulating or enhancing the body’s natural defense mechanisms, immunotherapy offers a unique way to combat metastatic breast cancer.
This section will provide a detailed overview of immunotherapy, its mechanisms of action, and different types of immunotherapy approaches.
The Role of the Immune System in Cancer:
The immune system plays a crucial role in recognizing and eliminating abnormal cells, including cancer cells.
However, cancer cells can develop strategies to evade the immune system’s surveillance and continue growing unchecked.
Immunotherapy aims to reactivate and strengthen the immune response against cancer cells, restoring the body’s ability to fight the disease.
Mechanisms of Action in Immunotherapy:
Immunotherapy employs various mechanisms to target cancer cells effectively. These mechanisms include:
Checkpoint Inhibition:
Checkpoint inhibitors are drugs that block specific proteins on immune cells or cancer cells, known as checkpoints.
By inhibiting these checkpoints, immunotherapy removes the “brakes” that cancer cells exploit to evade immune detection, allowing the immune system to recognize and attack the cancer cells more effectively.
Monoclonal Antibodies:
Monoclonal antibodies are laboratory-produced proteins that can specifically bind to certain molecules present in cancer cells.
They can directly interfere with cancer cell growth, and signaling pathways, or aid the immune system in recognizing and destroying cancer cells.
Adoptive Cell Therapy:
Adoptive cell therapy involves modifying a patient’s immune cells, such as T cells, outside the body to enhance their ability to target cancer cells.
These modified cells are then infused back into the patient, where they can seek out and destroy cancer cells more effectively.
Cancer Vaccines:
Cancer vaccines aim to stimulate the immune system’s response against cancer cells by introducing specific molecules or antigens found on the surface of cancer cells.
These vaccines can trigger the immune system to generate a targeted immune response against the cancer cells, helping to control tumor growth.

Types of Immunotherapy Approaches:
Immunotherapy encompasses various approaches tailored to activate the immune system against cancer. These approaches include:
Immune Checkpoint Inhibitors:
Immune checkpoint inhibitors, such as pembrolizumab and atezolizumab, block proteins like PD-1 or PD-L1, which are involved in suppressing immune responses.
By blocking these proteins, checkpoint inhibitors unleash the immune system’s ability to recognize and attack cancer cells.
Bispecific Antibodies:
Bispecific antibodies are designed to simultaneously bind to a target on cancer cells and immune cells.
By bringing these cells together, bispecific antibodies enhance the immune system’s ability to target and eliminate cancer cells.
Chimeric Antigen Receptor (CAR) T-cell Therapy:
CAR T-cell therapy involves modifying a patient’s own T cells to express a synthetic receptor called a chimeric antigen receptor.
This receptor enables the T cells to recognize and bind to specific proteins in cancer cells, leading to their destruction.
Oncolytic Viruses:
Oncolytic viruses are engineered viruses that can selectively infect and replicate within cancer cells, causing their destruction.
Additionally, these viruses can stimulate the immune system’s response against cancer cells, further enhancing the anti-tumor effect.
Immunotherapy Drugs for Metastatic Breast Cancer
Immunotherapy has emerged as a promising treatment option for metastatic breast cancer, offering new avenues for combating the disease.
This section will delve into the specific immunotherapy drugs developed for metastatic breast cancer, their mechanisms of action, and the targets they aim to exploit.
Checkpoint Inhibitors:
Checkpoint inhibitors, such as pembrolizumab and atezolizumab, have shown significant efficacy in treating metastatic breast cancer.
These drugs work by blocking specific proteins, such as PD-1 or PD-L1, which act as checkpoints on immune cells or cancer cells.
By inhibiting these checkpoints, checkpoint inhibitors unleash the immune system, allowing it to recognize and attack cancer cells more effectively.
Monoclonal Antibodies:
Monoclonal antibodies, like trastuzumab and pertuzumab, have been developed to target specific molecules present on cancer cells.
Trastuzumab, for instance, targets the HER2 protein found in HER2-positive breast cancer. Monoclonal antibodies can interfere with cancer cell growth, signaling pathways, or facilitate immune recognition and destruction of cancer cells.
Adoptive Cell Therapy:
Adoptive cell therapy involves modifying a patient’s immune cells, such as T cells, to enhance their ability to target cancer cells.
Chimeric Antigen Receptor (CAR) T-cell therapy is a notable example in this category. CAR T-cell therapy modifies a patient’s T cells to express a synthetic receptor called a chimeric antigen receptor.
This receptor enables the T cells to recognize and bind to specific proteins present on cancer cells, triggering their destruction.
Cancer Vaccines:
Cancer vaccines are designed to stimulate the immune system’s response against cancer cells. They can introduce specific molecules or antigens found on the surface of cancer cells, training the immune system to generate a targeted immune response against the cancer.
Vaccines such as the HER2 peptide vaccine have been developed for metastatic breast cancer to enhance immune recognition and attack against cancer cells.
Each of these immunotherapy drugs targets different aspects of metastatic breast cancer, utilizing the body’s immune system to mount a powerful defense against the disease.
By exploiting the mechanisms of action unique to each drug, they provide a targeted and personalized approach to treatment.
Read More: Melatonin Dose for Lung Cancer
Clinical Trials and Research Findings
Clinical trials play a crucial role in advancing our understanding of immunotherapy drugs for metastatic breast cancer. This section explores the significance of clinical trials and highlights some notable research findings in the field.
Importance of Clinical Trials:
Clinical trials are essential for evaluating the safety and efficacy of immunotherapy drugs in treating metastatic breast cancer.
These trials involve rigorous testing on human participants and provide valuable insights into the potential benefits and limitations of these treatments.
They help researchers identify optimal dosages, assess side effects, and determine which patient populations may benefit the most from immunotherapy.
Ongoing Clinical Trials:
Numerous clinical trials are currently underway to evaluate the effectiveness of immunotherapy drugs for metastatic breast cancer.
These trials aim to explore new drug combinations, investigate biomarkers that may predict treatment response, and assess the long-term outcomes of immunotherapy.
By participating in clinical trials, patients have the opportunity to access cutting-edge treatments and contribute to the advancement of knowledge in the field.
Research Findings:
Checkpoint Inhibitors:
Research studies have shown promising results for checkpoint inhibitors in metastatic breast cancer.
For example, the Keynote-012 trial demonstrated that pembrolizumab, a checkpoint inhibitor targeting PD-1, had encouraging response rates and improved survival in patients with advanced triple-negative breast cancer.
Monoclonal Antibodies:
Studies investigating monoclonal antibodies, such as trastuzumab and pertuzumab, have revealed significant benefits in HER2-positive metastatic breast cancer.
These antibodies, in combination with chemotherapy, have shown improved response rates and extended survival in clinical trials like the CLEOPATRA study.
Adoptive Cell Therapy:
Clinical trials focusing on CAR T-cell therapy have shown promising results in treating metastatic breast cancer. In a small study, CAR T-cell therapy targeting the protein MUC1 demonstrated objective responses and prolonged disease stabilization in patients with metastatic breast cancer.
Cancer Vaccines:
Research into cancer vaccines for metastatic breast cancer is ongoing. Early clinical trials evaluating vaccines targeting HER2 have shown promising immunological responses, although their impact on long-term survival is still being explored.
These research findings underscore the potential of immunotherapy drugs for metastatic breast cancer.
While further research is needed to refine treatment strategies and optimize patient selection, the results from clinical trials provide hope for improved outcomes and expanded treatment options in the future.

Efficacy and Side Effects
The efficacy and side effects of immunotherapy drugs for metastatic breast cancer are critical considerations in evaluating their overall impact on patient outcomes.
This section explores the efficacy of immunotherapy drugs and highlights common side effects associated with their use.
Efficacy of Immunotherapy Drugs:
Checkpoint Inhibitors:
Checkpoint inhibitors have demonstrated efficacy in subsets of patients with metastatic breast cancer.
For example, in clinical trials, checkpoint inhibitors have shown promising response rates and improved overall survival in patients with triple-negative breast cancer or those with tumors expressing high levels of PD-L1.
Monoclonal Antibodies:
Monoclonal antibodies targeting specific molecules, such as HER2, have shown substantial efficacy in HER2-positive metastatic breast cancer.
Combining these antibodies with chemotherapy has led to increased response rates, delayed disease progression, and improved overall survival compared to chemotherapy alone.
Adoptive Cell Therapy:
While still in the early stages of development, adoptive cell therapy, particularly CAR T-cell therapy, has demonstrated promising efficacy in certain subsets of patients with metastatic breast cancer.
Clinical trials have shown objective responses and disease stabilization in patients treated with CAR T-cell therapy targeting specific antigens.
Cancer Vaccines:
The efficacy of cancer vaccines for metastatic breast cancer is still under investigation, and more research is needed.
Early clinical trials have shown immunological responses, but their impact on long-term survival outcomes is yet to be fully determined.
Read More: Can Testicular Cancer Cause Birth Defects?
Common Side Effects:
Checkpoint Inhibitors:
Checkpoint inhibitors can cause immune-related adverse events (irAEs) due to their mechanism of action.
These irAEs may include fatigue, rash, diarrhea, endocrine abnormalities, and inflammation of various organs, such as the lungs (pneumonitis) or intestines (colitis). Prompt recognition and management of irAEs are crucial to minimizing their impact.
Monoclonal Antibodies:
Monoclonal antibodies generally have a favorable side effect profile. However, specific side effects may occur depending on the antibody used.
For example, monoclonal antibodies targeting HER2, such as trastuzumab, may be associated with cardiac toxicity or infusion-related reactions.
Adoptive Cell Therapy:
CAR T-cell therapy can lead to side effects known as cytokine release syndrome (CRS) and neurologic toxicities. CRS can cause flu-like symptoms, fever, low blood pressure, and in severe cases, organ dysfunction.
Neurologic toxicities may manifest as confusion, seizures, or difficulty speaking. Close monitoring and appropriate management are essential for patient safety.
Cancer Vaccines:
Cancer vaccines generally have a favorable side effect profile, with mild to moderate local reactions at the injection site being the most common. Systemic side effects are rare but may include flu-like symptoms or transient fatigue.
Combining Immunotherapy with Other Treatments
Combination therapy, involving the use of immunotherapy drugs alongside other treatment modalities, has emerged as a promising approach to enhance the effectiveness of immunotherapy in treating metastatic breast cancer.
This section explores the rationale behind combining immunotherapy with other treatments and highlights some notable strategies and their potential benefits.
The rationale for Combination Therapy:
Combining immunotherapy with other treatments aims to leverage the strengths of multiple modalities to achieve synergistic effects and improve treatment outcomes. The rationale for combining immunotherapy with other treatments includes:
Enhanced Immune Activation:
Certain treatments, such as chemotherapy or radiation therapy, can help create a more favorable immune microenvironment by reducing the tumor burden or promoting immune cell infiltration, thus enhancing the effectiveness of immunotherapy.
Overcoming Resistance:
Some tumors may develop resistance to immunotherapy or other treatments. Combining different modalities can target multiple pathways, making it more challenging for the tumor to evade treatment and reducing the likelihood of resistance.
Complementary Mechanisms of Action:
Immunotherapy and other treatments often have distinct mechanisms of action. Combining them can exploit different vulnerabilities of cancer cells, resulting in a more comprehensive and effective attack against the tumor.
Strategies for Combination Therapy:
Chemotherapy and Immunotherapy:
Combining chemotherapy with immunotherapy has shown promise in metastatic breast cancer. Chemotherapy can enhance immune responses by releasing tumor antigens and reducing immunosuppressive cells.
Additionally, certain chemotherapeutic agents, like nab-paclitaxel, have demonstrated synergistic effects when combined with checkpoint inhibitors.
Targeted Therapies and Immunotherapy:
Targeted therapies, such as HER2 inhibitors or CDK4/6 inhibitors, can be combined with immunotherapy drugs to capitalize on their respective strengths.
For example, combining HER2-targeted therapy with checkpoint inhibitors has shown improved response rates and prolonged survival in patients with HER2-positive metastatic breast cancer.
Radiotherapy and Immunotherapy:
Radiotherapy can promote immune responses by causing tumor cell death and releasing tumor antigens.
When combined with immunotherapy, radiotherapy can enhance the immune system’s ability to recognize and target cancer cells outside the radiation field, leading to improved local and distant tumor control.
Other Immunotherapy Combinations:
Combining different immunotherapy approaches, such as checkpoint inhibitors with adoptive cell therapy or cancer vaccines, is also being explored.
These combinations aim to engage multiple facets of the immune system, improving response rates and prolonging disease control.
Potential Benefits of Combination Therapy:
Combining immunotherapy with other treatments has the potential to yield several benefits, including:
Improved Response Rates:
Combination therapy has shown increased response rates compared to single-agent immunotherapy or other treatments alone.
This can lead to enhanced tumor control and improved outcomes for patients with metastatic breast cancer.
Prolonged Survival:
Some combination therapies have demonstrated improved overall survival compared to monotherapy. By targeting multiple pathways and vulnerabilities, combination treatments can overcome resistance mechanisms and extend patient survival.
Reduced Toxicity:
Combination therapies may allow for lower dosages of individual treatments, reducing the overall toxicity burden on patients while maintaining therapeutic efficacy.
Long-Term Disease Control:
The synergistic effects of combination therapy may result in prolonged disease control, delaying disease progression and providing patients with extended periods of tumor stability.
Conclusion
Immunotherapy drugs have emerged as a valuable addition to the treatment arsenal for metastatic breast cancer.
The development of checkpoint inhibitors, monoclonal antibodies, adoptive cell therapy, and cancer vaccines has opened new avenues for personalized and targeted treatment approaches.
Clinical trials and research findings have provided valuable insights into the efficacy of these immunotherapy drugs, highlighting their potential benefits in improving patient outcomes.
Combining immunotherapy with other treatments, such as chemotherapy, targeted therapies, or radiotherapy, offers a synergistic approach to maximize treatment efficacy.
By leveraging complementary mechanisms of action and enhancing immune activation, combination therapy has the potential to improve response rates, prolong survival, and achieve long-term disease control.
While immunotherapy has shown promise, it is crucial to be aware of potential side effects associated with these treatments.
Close monitoring and timely management of side effects are essential for patient safety and treatment continuity.
Overall, the field of immunotherapy for metastatic breast cancer is rapidly evolving, with ongoing research and clinical trials continuously refining treatment strategies and identifying novel combinations.
The future holds great promise for further advancements in immunotherapy, ultimately leading to improved outcomes for patients with metastatic breast cancer.
FAQs
Can immunotherapy drugs cure metastatic breast cancer?
Immunotherapy drugs have shown significant efficacy in treating metastatic breast cancer, but they may not cure the disease for all patients. The response to immunotherapy can vary among individuals, and additional research is needed to identify predictive biomarkers and optimize treatment strategies.
What are the side effects of immunotherapy for metastatic breast cancer?
Common side effects of immunotherapy can include fatigue, rash, diarrhea, endocrine abnormalities, pneumonitis, colitis, cardiac toxicity, infusion-related reactions, cytokine release syndrome, and neurologic toxicities. However, it is important to note that side effects can vary among individuals.
Can immunotherapy be used in combination with chemotherapy?
Yes, immunotherapy can be combined with chemotherapy to enhance treatment outcomes. Chemotherapy can enhance immune responses and create a more favorable immune microenvironment, synergizing with immunotherapy to improve efficacy.
What are the benefits of combining immunotherapy with targeted therapies?
Combining immunotherapy with targeted therapies, such as HER2 inhibitors or CDK4/6 inhibitors, can capitalize on their respective strengths. This combination approach has shown improved response rates and prolonged survival in patients with specific molecular subtypes of metastatic breast cancer.
How does immunotherapy enhance the immune system’s response against cancer?
Immunotherapy enhances the immune system’s response against cancer by blocking immune checkpoints, facilitating immune cell recognition and targeting of cancer cells, and stimulating the immune system through vaccines or adoptive cell therapy.
Are there ongoing clinical trials for immunotherapy in metastatic breast cancer?
Yes, numerous clinical trials are currently underway to evaluate the efficacy and safety of immunotherapy drugs, explore new combinations, identify predictive biomarkers, and optimize treatment approaches for metastatic breast cancer.
Can immunotherapy be used as a first-line treatment for metastatic breast cancer?
In certain cases, immunotherapy may be used as a first-line treatment for metastatic breast cancer, particularly in patients with specific molecular subtypes or high expression of targetable immune markers. However, the selection of treatment depends on several factors, and individualized treatment decisions should be made in consultation with healthcare providers.
Are there any long-term benefits of immunotherapy for metastatic breast cancer?
Immunotherapy has shown potential for providing long-term disease control in some patients with metastatic breast cancer. Combination therapies, in particular, have demonstrated extended periods of tumor stability and improved overall survival.
What is the future of immunotherapy for metastatic breast cancer?
The future of immunotherapy for metastatic breast cancer holds great promise. Ongoing research, clinical trials, and advancements in understanding the tumor microenvironment and immune responses will further optimize treatment strategies, identify predictive biomarkers, and expand treatment options for patients.
References
- Schmid P, Cortes J, Pusztai L, et al. Pembrolizumab for Early Triple-Negative Breast Cancer. N Engl J Med. 2020;382(9):810-821. doi:10.1056/NEJMoa1910549
- Emens LA, Esteva FJ, Beresford M, et al. Overall Survival Analysis of IMpassion130: A Phase III Study of Atezolizumab Plus Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. Cancer Cell. 2020;37(6):986-993.e5. doi:10.1016/j.ccell.2020.04.012
- Loi S, Giobbie-Hurder A, Gombos A, et al. Pembrolizumab plus trastuzumab in trastuzumab-resistant, advanced, HER2-positive breast cancer (PANACEA): a single-arm, multicentre, phase 1b-2 trial. Lancet Oncol. 2019;20(3):371-382. doi:10.1016/S1470-2045(18)30911-7
- Adams S, Schmid P, Rugo HS, et al. Pembrolizumab monotherapy for previously treated metastatic triple-negative breast cancer: cohort A of the phase II KEYNOTE-086 study. Ann Oncol. 2019;30(3):397-404. doi:10.1093/annonc/mdz012
- Emens LA, Adams S, Barrios CH, et al. LBA17 – IMpassion130: Final OS analysis from the pivotal phase III study of atezolizumab + nab-paclitaxel vs placebo + nab-paclitaxel in previously untreated locally advanced or metastatic triple-negative breast cancer. Ann Oncol. 2020;31:S1142-S1215. doi:10.1016/j.annonc.2020.08.2279
- Nanda R, Liu MC, Yau C, et al. Pembrolizumab plus standard neoadjuvant therapy for high-risk breast cancer (BC): results from I-SPY 2. J Clin Oncol. 2017;35(15_suppl):506. doi:10.1200/JCO.2017.35.15_suppl.506



